Introduction: A Pervasive Issue
Imagine a middle-aged man who once enjoyed morning walks in the park.
Over the years,
His knees began to ache, at first only after long activity, but eventually with every step. Painkillers gave him brief relief, physiotherapy helped for a while, and doctors told him surgery might be the “final option.”
For many, this is not just a story—it is daily reality.

Musculoskeletal disorders (MSDs) are among the most common health problems worldwide. They affect people of all ages—from young athletes sidelined by injuries to older adults struggling with degenerative diseases like osteoarthritis.
According to global health statistics,
MSDs are one of the leading causes of disability, reducing both quality of life and economic productivity.
What are MSDs?
Simply put, musculoskeletal disorders are conditions that affect the bones, joints, muscles, ligaments, and tendons—the very framework that allows us to move.
When any part of this system is injured or degenerates with age, it can cause pain, stiffness, swelling, and reduced mobility.
Common Conditions:
Osteoarthritis (OA)
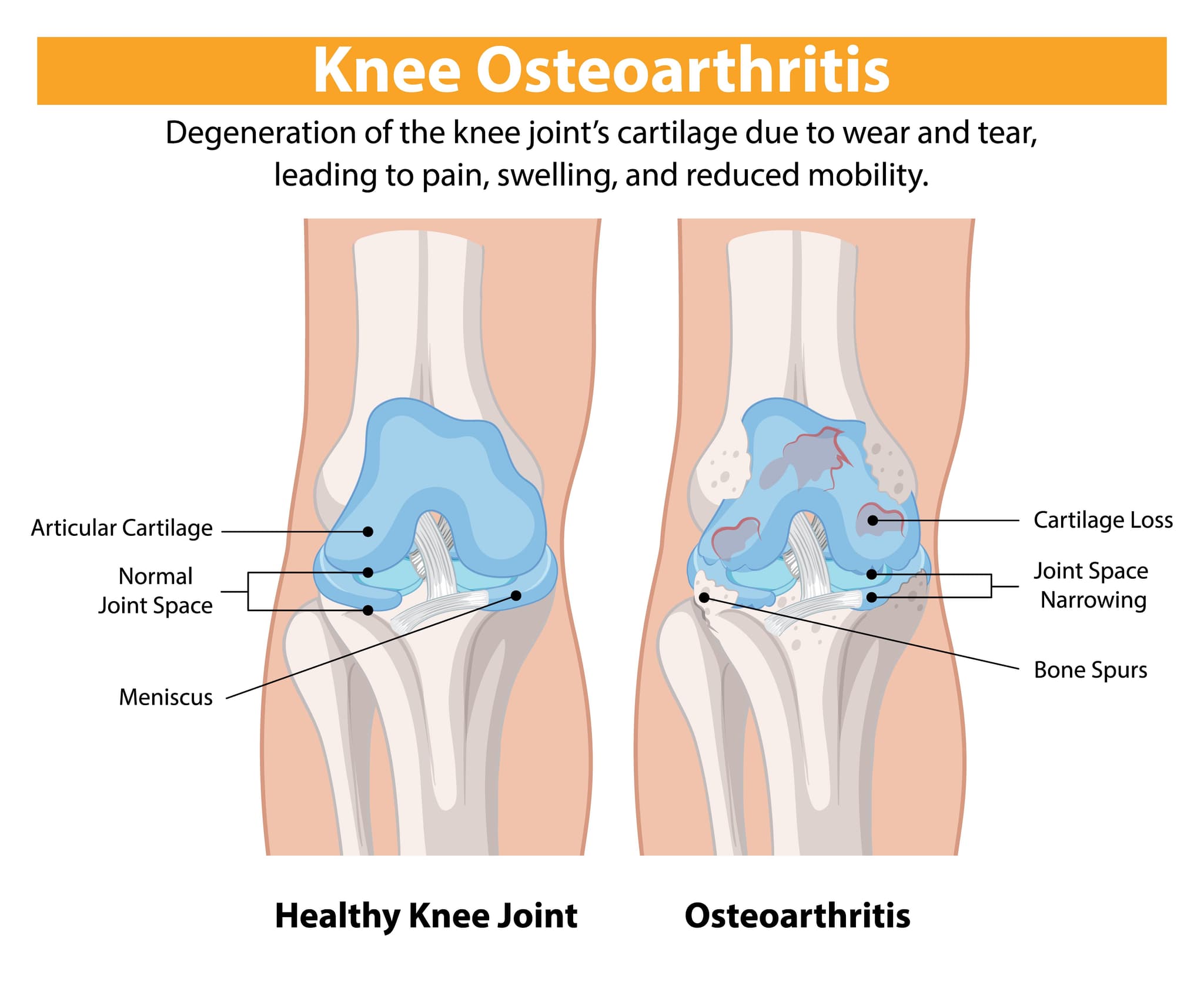
If you ask anyone over 50 what bothers them the most about their health, chances are you’ll hear: “My knees.” Osteoarthritis (OA) is one of the most common reasons people lose their mobility and independence as they age.
In fact,
According to the World Health Organization, more than 500 million people worldwide live with OA, making it one of the leading causes of disability.
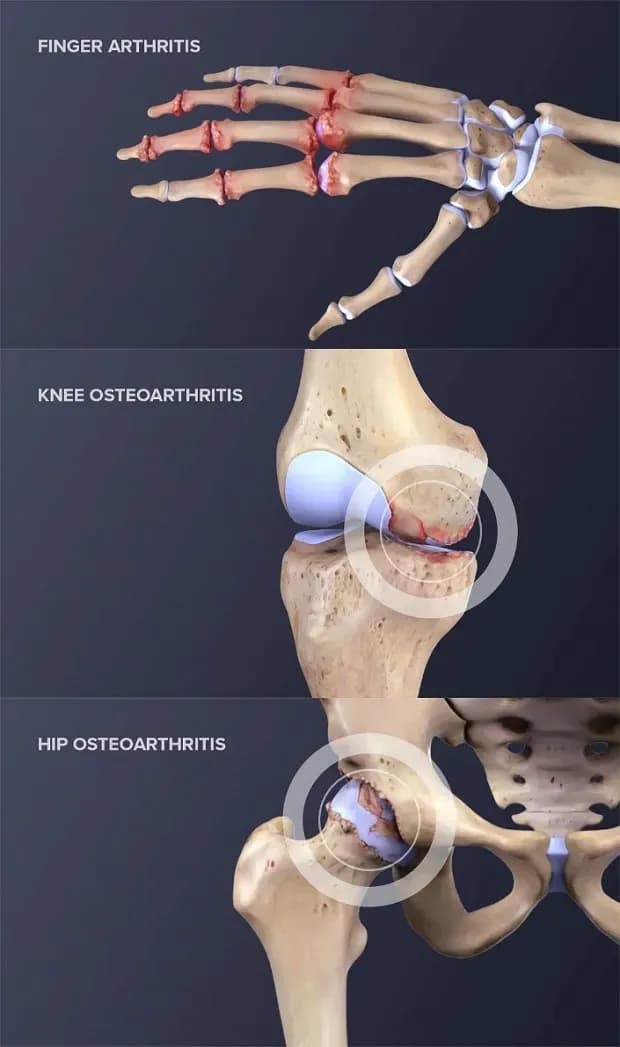
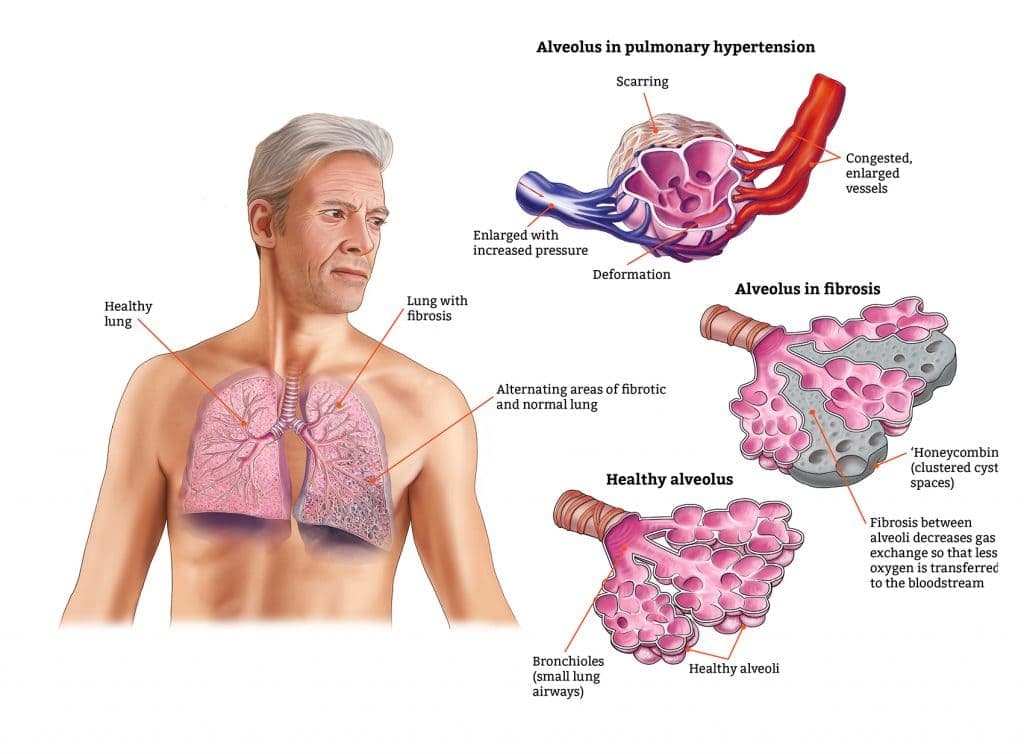
So, what exactly happens in osteoarthritis?
Imagine the cartilage in your knee joint as a smooth cushion that helps the bones glide against each other without friction.
Over time, with age, injury, or overuse, that cushion wears down.
As the cartilage thins, bones begin to grind against each other, causing pain, stiffness, swelling, and that unpleasant crunching sound many patients describe.
Daily activities— Climbing stairs, bending down to tie your shoes, or even enjoying a simple walk in the park—become painful chores.
Rheumatoid Arthritis (RA)
If osteoarthritis is the result of wear and tear, rheumatoid arthritis (RA) is more like your own body turning against itself.
For millions of people, RA is not just about sore joints—it’s a daily battle with fatigue, stiffness, and unpredictable flare-ups that disrupt work, family life, and even sleep.
RA is an autoimmune disease, which means the immune system—normally a protector—mistakenly attacks the body’s own tissues. In RA, the immune cells target the lining of the joints (synovium), causing painful inflammation, swelling, and eventually erosion of cartilage and bone. Patients often describe waking up with their fingers so stiff they can’t hold a toothbrush, or knees so swollen they struggle to get out of bed.
Over time, if uncontrolled, RA can lead to joint deformity and permanent disability.
Tendon & Ligament Injuries
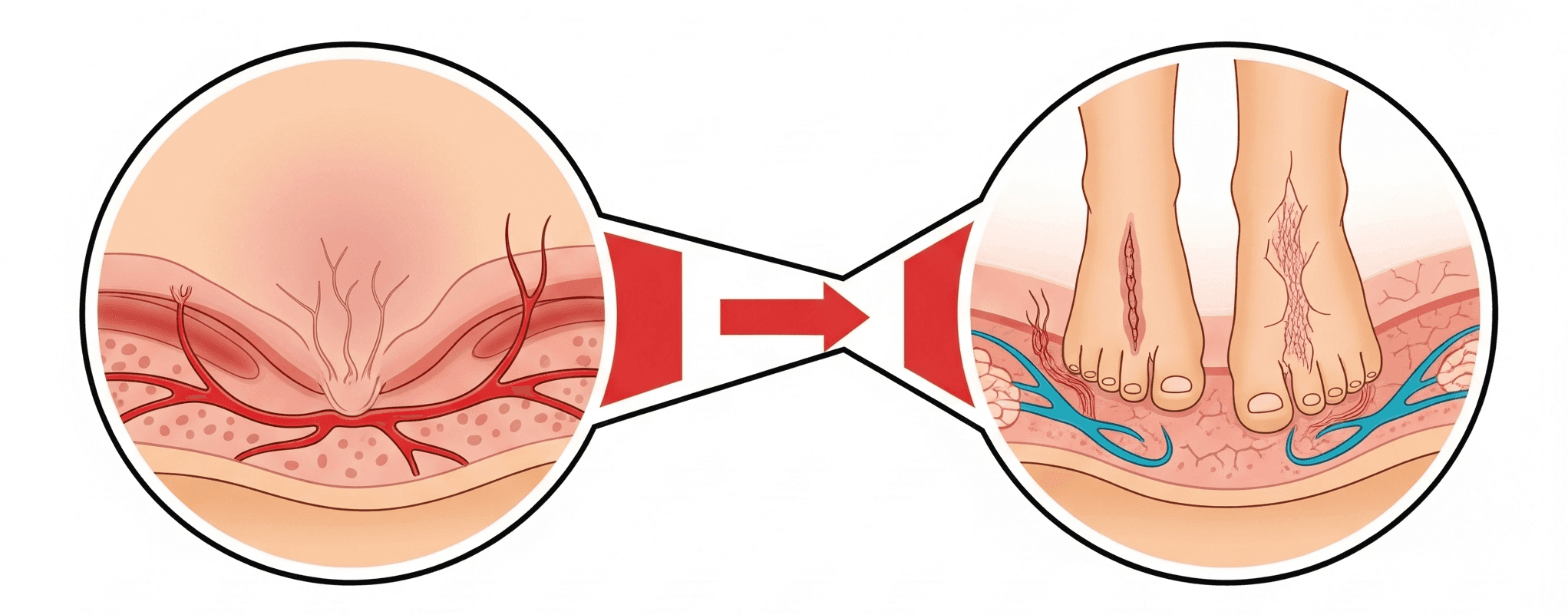
Think of tendons and ligaments as the wiring and ropes that hold our musculoskeletal system together.
Tendons connect muscle to bone, while ligaments connect bone to bone—keeping our joints stable and flexible.
When one of these structures tears, stretches too far, or degenerates, the results can be devastating. Common in athletes, these can take months to heal and often never fully regain original strength.
Unlike muscles, tendons and ligaments have very poor blood supply. This means when they’re injured, they heal slowly and often incompletely.
Common issues include: ACL tears (a nightmare for athletes), Rotator cuff injuries in the shoulder, Achilles tendon ruptures in runners, Chronic tendinopathies (like tennis elbow) that just won’t go away etc.
Back & Spinal Pain
Back pain—it’s often called the “silent epidemic.”
Almost everyone experiences it at some point, but for many, it becomes a constant companion, limiting movement, work, and even sleep. When it gets severe, it’s not just about discomfort; it can feel like life itself is on hold.
The spine is an engineering marvel—made of vertebrae, discs, nerves, muscles, and ligaments working together. But this complexity also means that pain can arise from many sources like Degenerative Disc Disease (DDD), Herniated Disc, Spinal Stenosis, Chronic inflammation or injury etc.
The impact of chronic pain is huge—not just physically but emotionally and socially.
People may give up sports, struggle to perform daily tasks, or feel isolated due to chronic pain. These conditions may start small but can progress into severe disability if not managed properly.
Limitations of Current Treatments
Traditional treatment options exist, but each has its drawbacks:
For most people struggling with chronic pain, the journey begins with the simplest solution: painkillers.
Tablets or capsules—sometimes over-the-counter, sometimes stronger—do offer temporary comfort. They take the edge off, make walking or sleeping a little easier, and provide the illusion of control. But the relief is fleeting.
The pain always returns, and over time, the body demands higher doses for the same effect. What was once a small pill for occasional pain turns into a daily dependency, with hidden costs like stomach irritation, kidney strain, or in the case of opioids, the looming shadow of addiction.
Physiotherapy is often introduced as the next step, and for good reason.
Targeted exercises, stretches, and movement training help patients preserve mobility and build the strength that joints so desperately need.
Many do find meaningful improvement—being able to climb stairs again, walk without limping, or enjoy activities that once felt impossible. But physiotherapy has its limits. When damage is advanced, when cartilage is already worn away, or when spinal structures have deteriorated, no amount of careful exercise can rebuild what has been lost.
The progress plateaus, leaving patients stuck in between temporary relief and lingering discomfort.
For quicker results, doctors sometimes recommend corticosteroid injections.
The promise is appealing—reduced swelling, less pain, and a chance to feel normal again. And indeed, for a few weeks or maybe a couple of months, patients often do feel better.
Yet the effect fades, and with each injection, the risks grow. Steroids are not gentle medicines; they can weaken tissues and accelerate degeneration if used repeatedly.
Instead of buying long-term healing, these injections often become short-lived bargains with the pain, always expiring too soon.
When all else fails, surgery looms as the final option.
Joint replacements and spinal operations can sound like miracles—cutting away the pain and starting fresh with new parts. And sometimes, they do restore lives.
But surgery is never a light decision. The recovery is long and difficult, the risks are real, and the outcomes are not always predictable. Even successful joint replacements come with an expiration date, because artificial implants do not last forever.
For younger patients, this means facing the likelihood of another major surgery years down the line, each one more complicated than the last.
The truth is,
Conventional treatments mostly focus on quieting symptoms, not curing the condition.
They provide comfort but rarely address the underlying damage. Patients often find themselves circling through pills, therapies, injections, and operations, chasing relief yet never truly healing. It is this gap—the space between managing pain and restoring health—that modern regenerative medicine is beginning to fill.
The Need for a New Approach
The current approach often manages symptoms rather than fixing the root problem.
What patients need is a therapy that not only eases pain but also heals damaged tissues and restores function naturally. This is where regenerative medicine—and specifically stem cell therapy—enters the picture as a game-changing solution.
What are Stem Cells?
Think of stem cells as the “master builders” of the body.
They are unspecialized cells capable of transforming into different types of specialized cells—like cartilage, bone, or muscle. Not only can they become other cells, but they can also self-renew, making copies of themselves to continue the repair process.
In other words, if your body is like a city, stem cells are the construction workers who repair damaged roads, rebuild broken bridges, and signal other workers to start fixing problems.
Different Types of Stem Cells
There are two main categories of stem cells relevant to medicine:
The Special Case of Umbilical Cord Stem Cells
Among the different sources of adult stem cells, human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) stand out as one of the most promising.
Here’s why:
Key Functions of Umbilical Cord Stem Cells
hUC-MSCs are not just repair cells—they are biological communicators.
They:
The Science Behind the Healing
When injected into damaged tissue, hUC-MSCs act as a repair crew.
Imagine a construction site after a storm:
This combined effect can restore joint function, reduce pain, and potentially halt or in cases reverse disease progression—something conventional medicine struggles to achieve.
The Treatment Process
Consultation & Diagnosis:
The journey begins with a detailed evaluation by a physician. Imaging studies (like MRI or X-rays) and physical exams confirm the extent of damage.
The Stem Cell Product:
hUC-MSCs are carefully prepared in advanced laboratories. Institutions like Concord Stem Cell in Bangladesh, DGDA-approved, cGMP-compliant stem cell manufacturer, ensure safety, quality, and reproducibility.
The Injection Procedure:
Using a minimally invasive approach, stem cells are injected directly into the affected joint (knee, hip, or shoulder). Guided by imaging, the doctor ensures precise placement.
Recovery & Response:
Unlike surgery, there’s little to no downtime. Patients often return to daily activities within a day or two. The real healing happens gradually over weeks to months as stem cells integrate and stimulate repair.
Case Studies / Applications
Difference from Traditional Methods
In short, it’s not just about living with less pain—it’s about restoring life and movement.
Pioneering the Future
Concord Stem Cell Limited is Bangladesh’s first DGDA-approved, cGMP-compliant stem cell manufacturing and treatment center, leading the nation into a new era of regenerative medicine and cell-based therapies. Situated in Dhaka, the facility is equipped with state-of-the-art ISO-7 and ISO-8 cleanrooms, ensuring the highest standards of safety, reproducibility and robust QC as per global benchmarks.
What truly sets Concord Stem Cell Limited apart is its commitment to innovation, ethical practices, and accessibility.
By bringing advanced regenerative medicine to Bangladesh, they eliminate the need for costly overseas treatments, making world-class healthcare locally available and affordable. Their mission is to harness the body’s own healing potential, reduce dependency on long-term medication, and offer natural, sustainable recovery solutions.
Commitment to Quality
Every batch of hUC-MSCs undergoes strict testing for safety, quality, and reproducibility.
The laboratory is staffed by experienced scientists and clinicians who ensure patients receive the highest-quality therapeutic products.
Accessibility and Vision
For years, patients had to travel abroad for regenerative therapies. Now, Concord is making them accessible at home—safe, ethical, and affordable. Their vision goes beyond treatment; it’s about restoring hope and quality of life for people who once thought surgery or lifelong pain were their only options.
The Future of Healing
Their vision extends beyond just joint therapy.
By pioneering in this field, Concord is paving the way for stem cell applications in neurology, cardiology, autoimmune diseases, and more—bringing new hope to conditions once labeled “incurable.”
Summary of Key Points
The Promise of a New Dawn
For people like Rafiq—and millions more—this therapy represents more than just pain relief. It’s about regaining independence, returning to activities they love, and experiencing a life free from constant discomfort.
This is not a distant dream. It’s happening now, and it’s changing lives.
If you or someone you love suffers from chronic joint pain, don’t settle for “managing” symptoms.
Explore regenerative options, consult with experts, and take proactive steps toward recovery. The future of healing is here—and it begins with awareness.